Overview
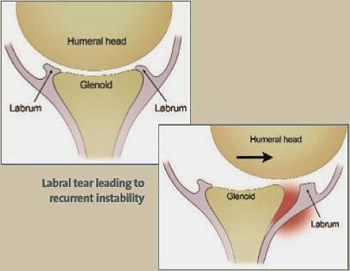
Shoulder instability is classified into two categories: subluxations and dislocations. To understand each, we must first understand the shoulder anatomy. The shoulder is a ball-and-socket joint comprised of the humerus (ball) and glenoid or glenoid fossa (socket). The glenoid is a shallow groove which comes off the scapula (shoulder blade) that articulates with the head of the humerus. Due to the glenoid’s shallow groove, the head of the humerus can become dislocated due to a direct force or if the shoulder is severely unstable, the shoulder can dislocate on its own.
A subluxation is: When an unstable shoulder can slip in and out of the joint. When subluxation occurs the shoulder is partially or not completely dislocated. If the shoulder is partially out of the shoulder socket, it may completely dislocate. Subluxations typically reduce on their own.
A dislocation is: When the head of the humerus comes completely out of the glenoid. One occurrence can lead to the condition known as chronic instability, where the shoulder is at a higher risk of subluxation and/or dislocation. Typically with shoulder dislocations, the labrum— the cartilage lining the glenoid— is often torn.
What Causes Shoulder Instability?
- A strong force applied to the shoulder
- Extreme rotation
- A hit while playing a contact sport
- A car accident
- Falling on an out-stretched arm
- A combination or multiple episodes of any of these mechanisms
Symptoms:
These are the most common symptoms of Shoulder Instability and Dislocations:
- General instability
- When in certain situations, evident apprehension or fear of repeating the dislocation
- Intense shoulder pain
- Numbness that radiates down the arm
- Visual deformity
- Asymmetric appearance in comparison to other shoulder
The Facts on Shoulder Instability and Dislocations:
- Shoulder instability is classified into two categories: subluxations and dislocations
- Typically with shoulder dislocations, the labrum— the cartilage lining the glenoid— is often torn
- Having weak surrounding muscles puts shoulders at a higher risk for chronic instability
- Treatment may include immobilization, medication, rehabilitation, or surgery
Evaluation by Team Ahmad
Dr. Ahmad and his team of health professionals will greet you and start your visit with a discussion of your symptoms.
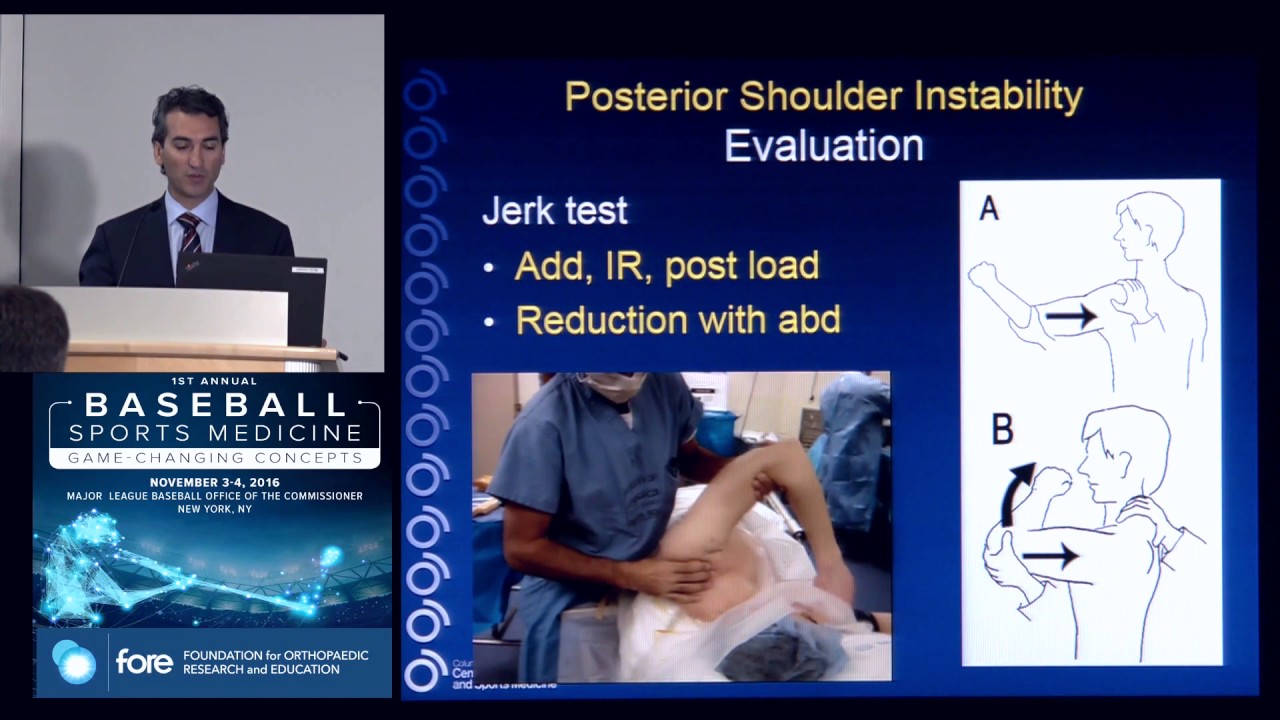
Next, the doctor will exam your shoulder, focusing on:
- How your shoulder was injured
- Pain points and reported levels of pain
- The range of motion of each shoulder
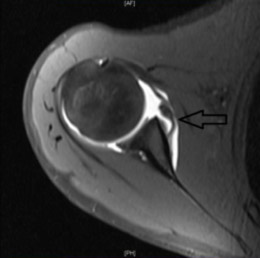
- If necessary, Dr. Ahmad may request an imaging scan, like an X-Ray or MRI,
- so he may better determine the extent of your injury.
- In extreme cases, a CT scan may be required.
Treatment Options
If you are experiencing intense shoulder pain or feelings of instability, you may require treatment to repair and prevent any damage. You should cease all strenuous activity and make an appointment with your doctor immediately. Treatment may include immobilization,medication,rehabilitation, or surgery.
Non-surgical
If you are experiencing intense shoulder pain or feelings of instability, you may require treatment to repair and prevent any damage. You should cease all strenuous activity and make an appointment with your doctor immediately. Treatment may include immobilization,medication,rehabilitation, or surgery.
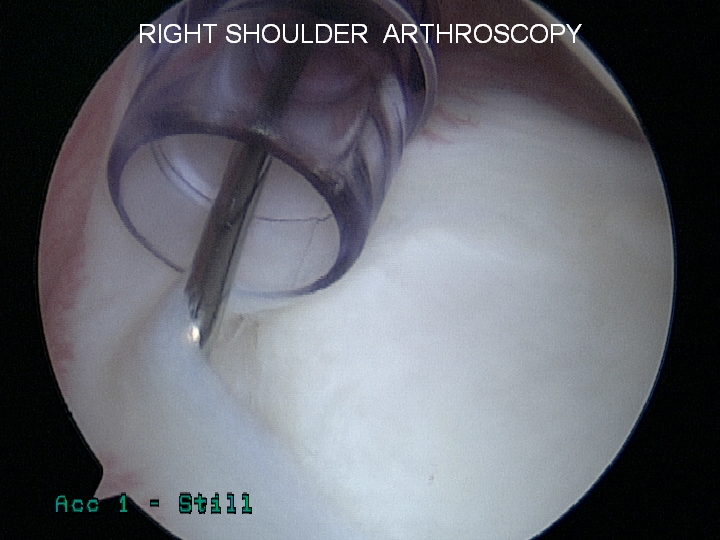
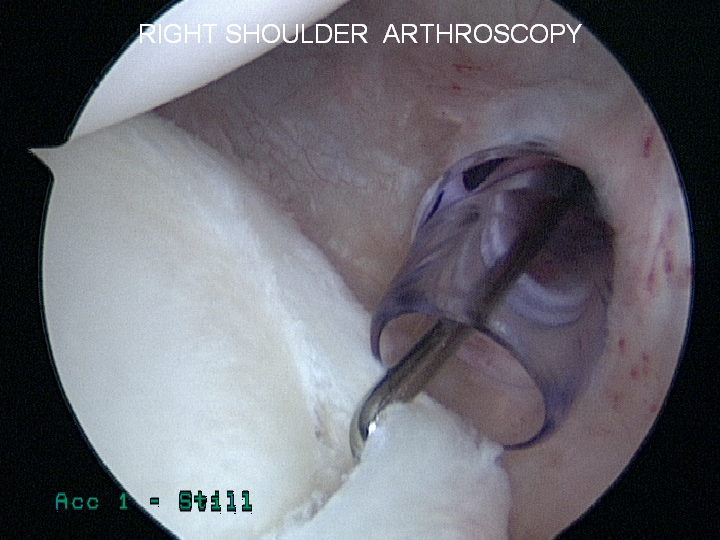
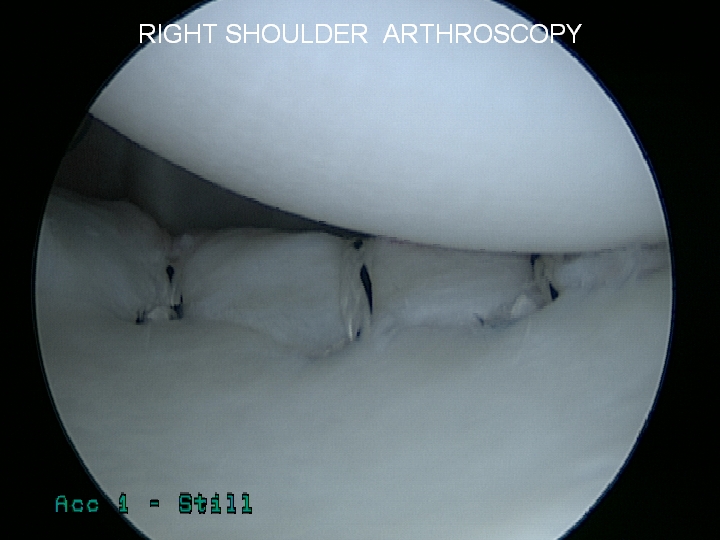
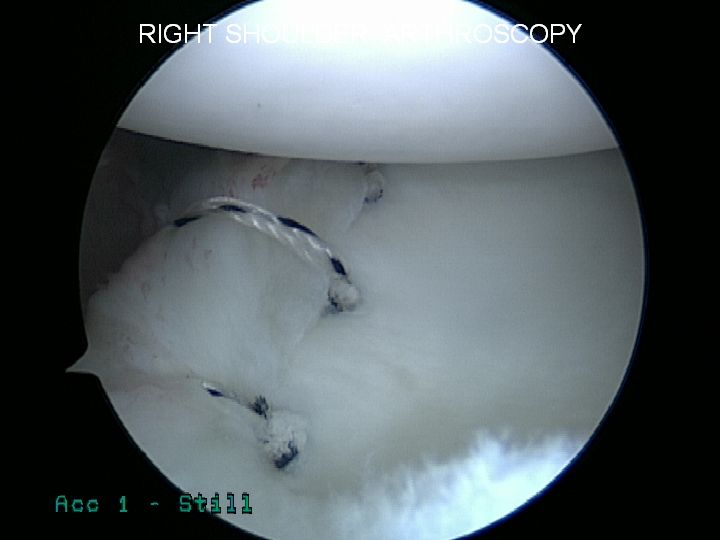
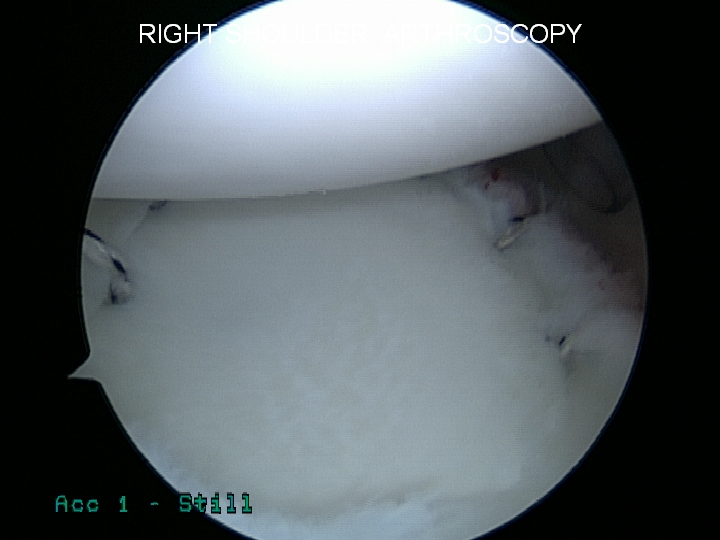
Surgical
Treatment for shoulder instability is circumstantial, and
depends on the severity of your injury and condition.
General treatment includes:
- Immobilization of the shoulder
- Medication (oral or injections)
- Rehabilitation
Rehabilitation and Recovery
After surgery, a sling is needed for roughly 4 to 6 weeks, and physical therapy starts after your first post-operative appointment.